By Aneri Pattani | KHN.org
The nurses at Mission Hospital in Asheville, North Carolina, declared on March 6 — by filing the official paperwork — that they were ready to vote on the prospect of joining a national union. At the time, they were motivated by the desire for more nurses and support staff, and to have a voice in hospital decisions.
A week later, as the covid-19 pandemic bore down on the state, the effort was put on hold, and everyone scrambled to respond to the coronavirus. But the nurses’ long-standing concerns only became heightened during the crisis, and new issues they’d never considered suddenly became urgent problems.
Staffers struggled to find masks and other protective equipment, said nurses interviewed for this story. The hospital discouraged them from wearing masks one day and required masks 10 days later. The staff wasn’t consistently tested for covid and often not even notified when exposed to covid-positive patients. According to the nurses and a review of safety complaints made to federal regulators, the concerns persisted for months. And some nurses said the situation fueled doubts about whether hospital executives were prioritizing staff and patients, or the bottom line.
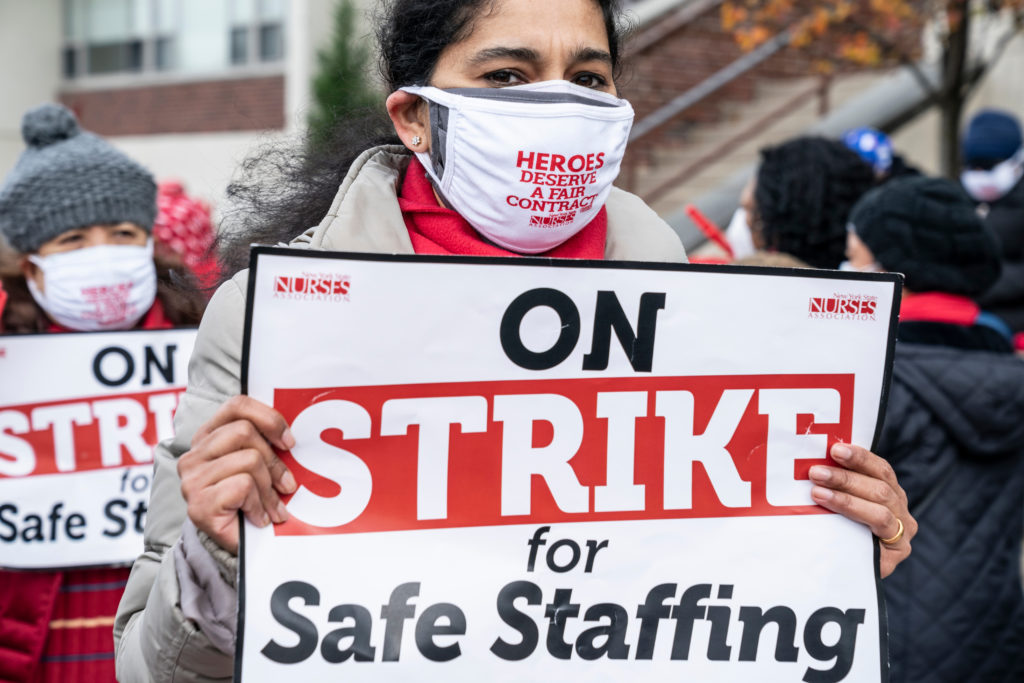
By the time the nurses held their election in September — six months after they had filed paperwork to do so — 70% voted to unionize. In a historically anti-union state with right-to-work laws and the second-least unionized workforce in the country, that margin of victory is a significant feat, said academic experts who study labor movements.
That it occurred during the pandemic is no coincidence.
For months now, front-line health workers across the country have faced a perpetual lack of personal protective equipment, or PPE, and inconsistent safety measures. Studies show they’re more likely to be infected by the coronavirus than the general population, and hundreds have died, according to reporting by KHN and The Guardian.
Many workers say employers and government systems that are meant to protect them have failed.
Research shows that health facilities with unions have better patient outcomes and are more likely to have inspections that can find and correct workplace hazards. One study found New York nursing homes with unionized workers had lower covid mortality rates, as well as better access to PPE and stronger infection control measures, than nonunion facilities.
Recognizing that, some workers — like the nurses at Mission Hospital — are forming new unions or thinking about organizing for the first time. Others, who already belong to a union, are taking more active leadership roles, voting to strike, launching public information campaigns and filing lawsuits against employers.
“The urgency and desperation we’ve heard from workers is at a pitch I haven’t experienced before in 20 years of this work,” said Cass Gualvez, organizing director for Service Employees International Union-United Healthcare Workers West in California. “We’ve talked to workers who said, ‘I was dead set against a union five years ago, but covid has changed that.’”
In response to union actions, many hospitals across the country have said worker safety is already their top priority, and unions are taking advantage of a difficult situation to divide staff and management, rather than working together.
Labor experts say it’s too soon to know if the outrage over working conditions will translate into an increase in union membership, but early indications suggest a small uptick. Of the approximately 1,500 petitions for union representation posted on the National Labor Relations Board website in 2020, 16% appear related to the health care field, up from 14% the previous year.
In Colorado, SEIU Local 105 health care organizing director Stephanie Felix-Sowy said her team is fielding dozens of calls a month from nonunion workers interested in joining. Not only are nurses and respiratory therapists reaching out, but dietary workers and cleaning staff are as well, including several from rural parts of the state where union representation has traditionally been low.
“The pandemic didn’t create most of the root problems they’re concerned about,” she said. “But it amplified them and the need to address them.”
A nurse for 30 years, Amy Waters had always been aware of a mostly unspoken but widespread sentiment that talking about unions could endanger her job. But after HCA Healthcare took over Mission Health in 2019, she saw nurses and support staff members being cut and she worried about the effect on patient care. Joining National Nurses United could help, she thought. During the pandemic, her fears only worsened. At times, nurses cared for seven patients at once, despite research indicating four is a reasonable number.
In a statement, Mission Health said it has adequate staffing and is aggressively recruiting nurses. “We have the beds, staffing, PPE supplies and equipment we need at this time and we are well-equipped to handle any potential surge,” spokesperson Nancy Lindell wrote. The hospital has required universal masking since March and requires staff members who test positive to stay home, she added.
Although the nurses didn’t vote to unionize until September, Waters said, they began acting collectively from the early days of the pandemic. They drafted a petition and sent a letter to administrators together. When the hospital agreed to provide advanced training on how to use PPE to protect against covid transmission, it was a small but significant victory, Waters said.
“Seeing that change brought a fair number of nurses who had still been undecided about the union to feel like, ‘Yeah, if we work together, we can make change,’” she said.
Old Concerns Heightened, New Issues Arise
Even as union membership in most industries has declined in recent years, health workers unions have remained relatively stable. Experts say it’s partly because of the focus on patient care issues, like safe staffing ratios, which resonate widely and have only grown during the pandemic.
The story continues at khn.org.
Editorial credit: lev radin / Shutterstock.com